Medical billing codes classify patients’ diagnosis, treatments, procedures and drug sets . Two essential billing coding systems involved in the billing are Current Procedural Terminology (CPT) codes and International Classification of Diseases (ICD) codes. These codes are mandatory for a clinician to reimburse for their services by private insurance companies or Medicaid or state-sponsored insurance plans. Let us explore further these key billing codes and their significance.
CPT Codes
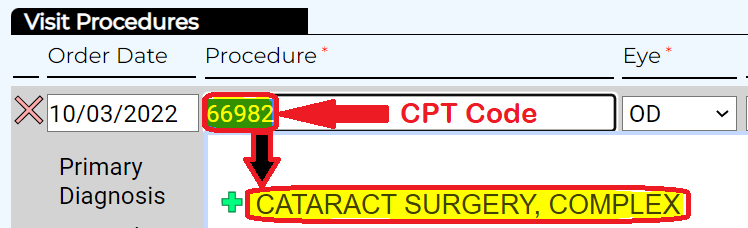
CPT Code
CPT codes or Current Procedural Terminology codes describe clinical procedures performed on a patient. Both the providers and payers use these codes to communicate the services rendered, billed, and paid for. The American Medical Association (AMA) created CPT codes to facilitate and standardize medical billing practices. They are widely used by US federal government programs like Medicare and Medicaid as well as private insurance companies.
They are one of the unique codes to analyze, diagnose, investigate, and provide services an individual or a patient has undergone when they go through medical appointments. CPT is represented as a language between the provider’s office and the insurance office which accept the medical bills.
ICD codes
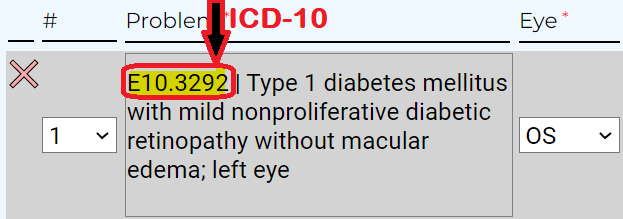
ICD Code
ICD codes, or International Classification of Disease codes, describe the medical diagnosis. In other words, they refer to the condition that’s being treated. The (ICD) coding system is a method of converting medical terminology into numerical codes. It is a code system that includes codes for illnesses, symptoms, abnormal findings, situations, and external causes of injury or disease. ICD codes can also identify health and disease trends across countries.
ICD codes are developed by the World Health Organization (WHO) and used worldwide.
The ICD-10 code system was introduced to keep up with the advanced healthcare and information technology industries.
How do CPT and ICD Codes Expedite Billing?
The codes are an essential part of the medical billing process. The two quickly provide payors with specific information describing the insurance payer, services and procedures performed on patients (the CPT code), and why (the ICD code). It also shows the exact charges for services.
Implementing the ICD-10 code set also enables more accurate payment for the latest techniques, fewer rejected claims, fewer fraudulent claims, a deeper understanding of procedures, and better disease control.
How to Submit the Codes?
When you implement the best ophthalmology EMR like Doctorsoft, the software automatically generates the codes as you enter the data of each service given during the consultation. The sequences in the process comprise of:
Submission
The healthcare providers submit the medical documents to the billing service. They review the documentation, assign codes, and forward the claim to the appropriate insurance firms.
Verification
The insurance firm verifies the claim and further reconfirms with the provider the covered services.
Claim Process
Once the verification is authenticated, the insurance firms process the claim and initiate the payment. Medical billing is a complex process. Doctorsoft offers a comprehensive and user-friendly Ophthalmology EHR and Revenue Cycle Management (RCM)) that can help your practice simplify its coding and billing process. A well-equipped expert panel manages all provider billing aspects, from claim submission to denial management.
Are you considering boosting your practice’s revenue and reducing denials? Reach out to us today.

Pingback: Doctor Soft (doctorsoft2k23) | Pearltrees