Why Is MIPS Important?
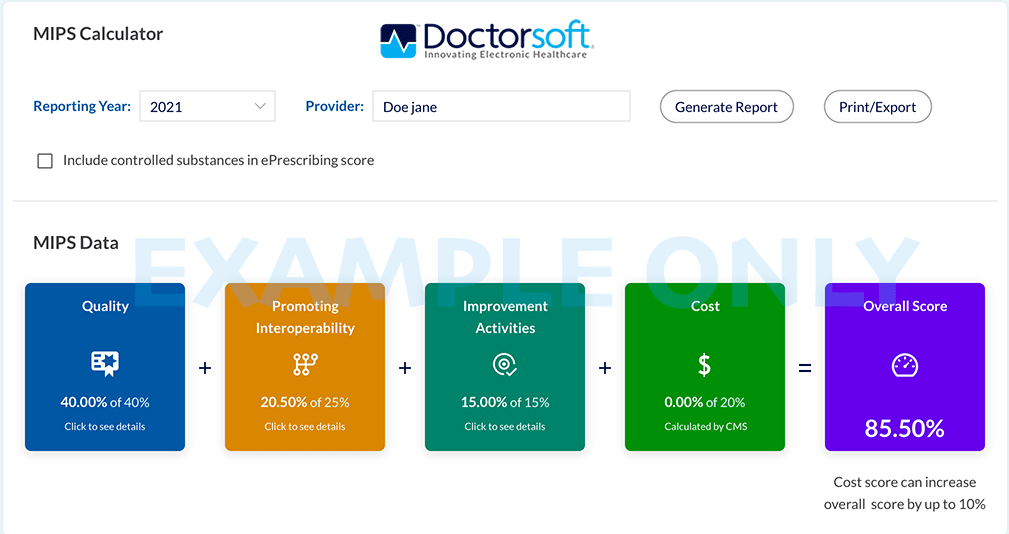
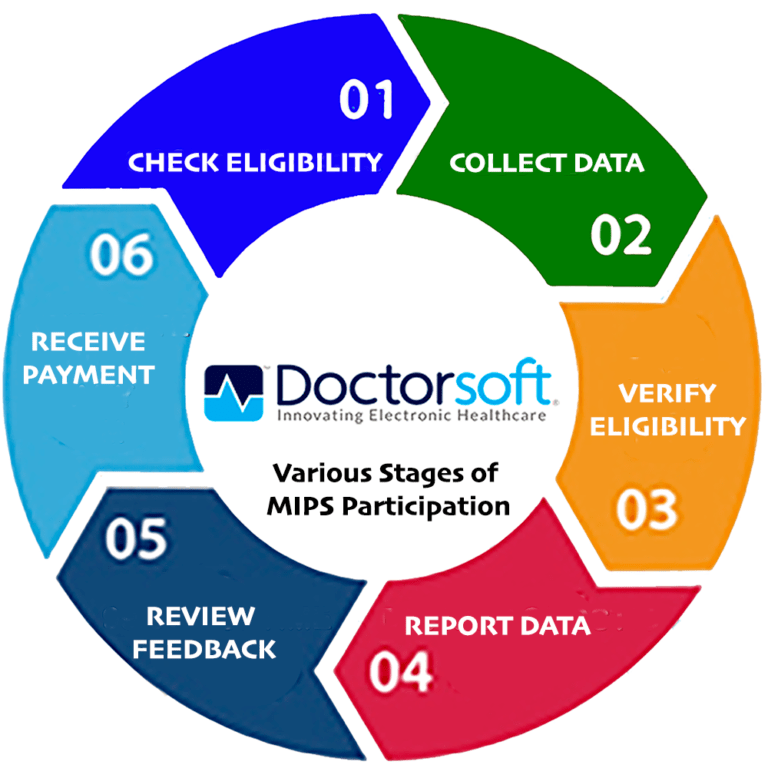
The Merit-Based Incentive Payment (MIPS) score determines an eligible physician’s MIPS final score, which is directly related to the dollar payout from Medicare, as well as, associated bonuses, penalties, or no payments. The quality measures and activities must be reported during the performance period or every quarter. CMS evaluates the measures and subsequently calculates your final MIPS score, which then determines the final payout.
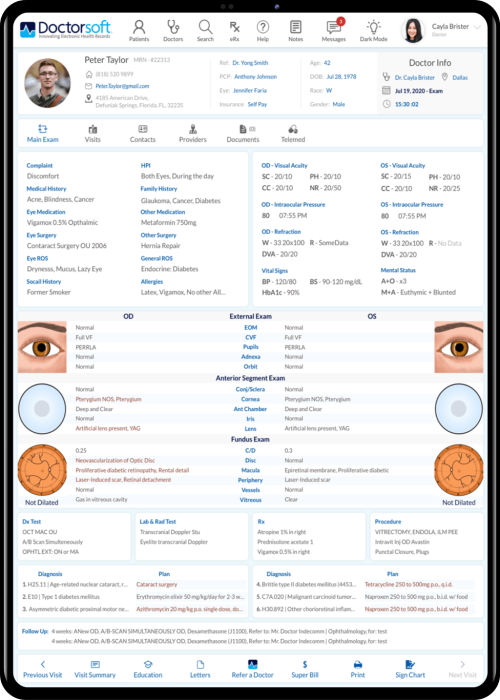
Doctorsoft ophthalmic EHR for a decade now continues to report the measures by seamlessly collecting the available data and reporting it at NO EXTRA charge.
Why Doctorsoft
No gimmicks! No extra charges! Just simple, straightforward reporting of your MIPS measures and activities. The backbone behind this automated process is robust state-of-the-art technology that removes the guessing game for practices.
What are the MIPS weighted performance categories?
Performance is measured through the data clinicians report in four areas:
This performance category replaces PQRS. This category covers the quality of the care you deliver, based on performance measures created by CMS, as well as medical professional and stakeholder groups. You pick the six measures of performance that best fit your practice.
1. Primary Open-Angle Glaucoma (POAG): Optic Nerve Evaluation.
2. Age-Related Macular Degeneration (AMD): Dilated Macular Examination.
3. Diabetic Retinopathy: Communication with the Physician Managing Ongoing Diabetes Care.
4. Diabetes: Eye Exam.
5. Primary Open-Angle Glaucoma (POAG):Reduction of Intra-ocular pressure.
6. Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention.
7. Documentation of Current Medications in the Medical Record.
8. Cataracts: 20/40 or Better Visual Acuity within 90 Days Following Cataract Surgery.
9. Use of High-Risk Medications in the Elderly.
10. Closing the Referral Loop: Receipt of Specialist Report.
11. Adult Primary Rhegmatogenous Retinal Detachment Surgery: No Return to the Operating Room Within 90 Days of Surgery.
12. Adult Primary Rhegmatogenous Retinal Detachment Surgery: Visual Acuity Improvement Within 90 Days of Surgery.
13. Cataract Surgery: Difference Between Planned and Final Refraction.
CMS is renaming the Advancing Care Information performance category to Promoting Interoperability (PI) to focus on patient engagement and the electronic exchange of health information using (CEHRT). This performance category replaced the Medicare EHR Incentive Program for EPs, commonly known as Meaningful Use. This is done by proactively sharing information with other clinicians or the patient in a comprehensive manner. This may include: sharing test results, visit summaries, and therapeutic plans with the patient and other facilities to coordinate care.
This is a new performance category that includes an inventory of activities that assess how you improve your care processes, enhance patient engagement in care, and increase access to care. The inventory allows you to choose the activities appropriate to your practice from categories such as, enhancing care coordination, patient and clinician shared decision-making, and expansion of practice access.
This performance category replaces the VBM. The cost of the care you provide will be calculated by CMS based on your Medicare claims. MIPS uses cost measures to gauge the total cost of care during the year or during a hospital stay. Beginning in 2018, this performance category will count towards your MIPS final score.
Doctorsoft IT solutions has designed MIPS to update and consolidate previous programs, including: Medicare (EHR) Incentive Program for Eligible Clinicians, (PQRS), and the Value-Based Payment Modifier program(VBM).
MIPS And MACRA
The Medicare Access and CHIP Reauthorization Act (MACRA) act in 2015, when it became law, immediately shifted the thought process towards a focus on medical payments.
CMS is required by law to implement a quality payment incentive program, referred to as the Quality Payment Program. This program rewards practices/physicians who provide high quality, low-cost care and penalizes those who don’t abide by the rules and fail to provide critical information regarding the aforementioned four measures and activities that ultimately determine the final MIPS score.
How are MIPS measures practiced by Doctorsoft?
- Security Risk Analysis
- E-Prescribing
- Sending Health Information
- Receiving Health Information
- Provide Patients Electronic Access

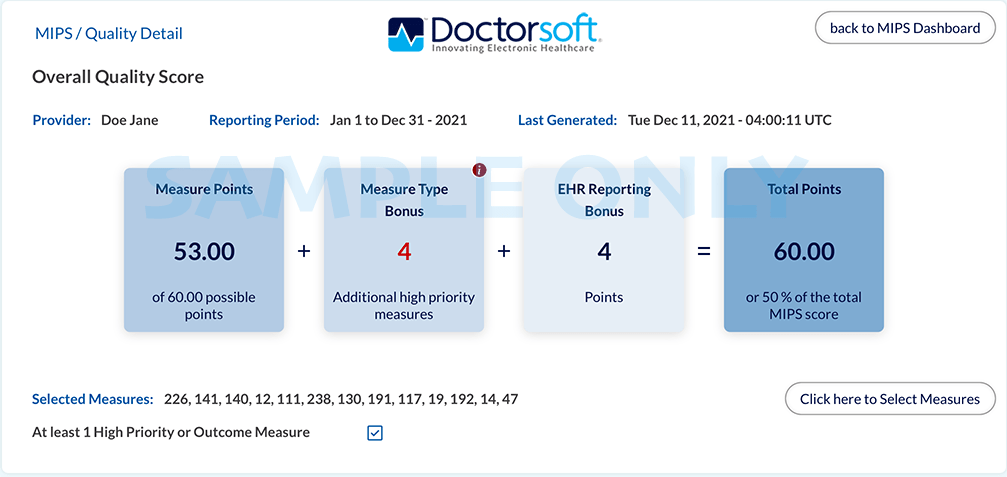
- A measure that has less than 20 eligble cases, can earn a maximum of 3 points.
- A low calculated performance rate for this measure indicates better clinical and care.
- A measure that is included in scoring examination.
- Measure not eligible for EHR reporting bonus.
How does Doctorsoft submit MIPS data to CMS?
Doctorsoft sends a practice’s data every month on time to the CMS (Centers for Medicare and Medicaid Services) through an alliance with a trusted third party registry. The third party registry securely and under strict compliance oversight transfers quality data (Promoting Interoperability and Improvement Activities) measures to the CMS. The IRIS registry plays a crucial role in the mapping of MIPS data and quality measures to third party decision makers at no cost to the practice.